By Marc Erickson, MD
CardioSmart Contributor
“Mr. G,” a 60-year-old burly white male who works as a mechanic, arrived at the cardiology fellows’ clinic by himself. He hails from a mountainous region of north Georgia and went into the valley of Chattanooga, rather than drive into metro Atlanta for medical care. He is married to a medical assistant and has some tangential medical knowledge, but he lets me know at the beginning of the visit he prefers to defer decisions on his medical care to his wife.
As a white male, also from Georgia – who has done both his internal medicine and cardiology fellowship in Chattanooga – I am familiar with this type of decision-making arrangement. Mr. G has a history of permanent atrial fibrillation diagnosed 22 years ago. He has been anticoagulated with warfarin since. He was referred to the clinic for assistance managing his atrial fibrillation, specifically his anticoagulation.
Mr. G ultimately came in to satisfy his wife. She is concerned that he could have bleeding complications or a stroke while he remains on warfarin. As he sees it, he has regulated his diet to keep his blood tests stable (maintain a consistent INR), and he has done well on the medication. Why change what has worked for more than 20 years?
Collaborative communication
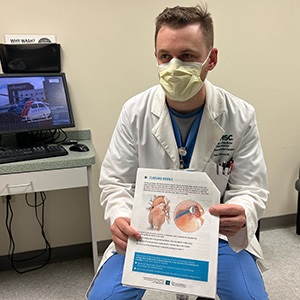
I use the decision aid for AFib with most of my patients who have that condition. It gives me a standardized starting place for me and my patients to build on. Going through the decision aid, he had a couple questions regarding anatomy and physiology: Where is the left atrial appendage? Why does it form clots? What is AFib? The handout helps with some of these questions but does not provide enough clarity regarding the rhythm or relevant anatomy. I fill in these gaps with my own theatrics in pantomiming the quivering of the atria, or the tract a thrombus might traverse.
He understands the risk of stroke. He has seen it in his own family. That is why he has remained on warfarin all these years. Regarding the risk of stroke, he proudly notes he is in the column of people who are on treatment. We continue through the table comparing warfarin and direct oral anticoagulants (DOACs); this is the crux of our visit today. We linger in silence on this table.
Doctors spend so much time talking, recommending, and prescribing that when we let stillness settle in the room, we convey that something new is happening. The power dynamic in the physician-patient relationship has classically been weighted toward the physician. We give up paternalism for a moment to see what will come forth and fill the void. This arrangement of unstable equilibrium can prompt great insight from the patient as they are given the power to lead the conversation.
Listen to what matters
As a mechanic Mr. G gets dinged, bruised, and cut, but the risks between warfarin and DOAC of bleeding are presented identically. The cost is what sticks out to him. His work is lucrative but offers no insurance, which is why he is here in the fellows’ clinic. He recalls being prescribed one of these newer medications years ago, but he was unable to afford them.
For him it is not about efficacy, but reliability. Reliability of his medical regimen, his diet, his doctors, and his work has kept him on warfarin. Like an engine timing the fall of pistons, predictability is his guiding virtue.
While cost is only briefly mentioned in the handout, it becomes the core of our discussion for the rest of the visit including the capability of our clinic and pharmacy to prescribe and refill this medication. Luckily at our institution, our pharmacy provides these medications at a significantly reduced cost.
By the end of our 30-minute visit, he decides to stay on warfarin, but he is willing to take the pamphlet home to his wife. At his next appointment, he comes in ready to be transitioned to a DOAC.
Marc Erickson, MD, is a first year fellow in cardiovascular disease at Erlanger Heart and Lung Institute in Chattanooga, TN.